Schauplatz Indien: Schwerstkranke Covid-Patienten teilen sich zu zweit ein Bett. Viele werden gar nicht behandelt. Angehörige verzweifeln an der Suche nach Sauerstoff. Leichen werden vor den überlasteten Krematorien auf Parkplätzen verbrannt. Bilder wie diese gingen vor allem im April und Mai um die Welt, auf dem Subkontinent zeigte sich die Corona-Pandemie von ihrer furchtbarsten Seite. Die Lage in Indien ist dabei auch auf die dort aufgetretene hochansteckende Delta-Variante des Coronavirus zurückzuführen. Mittlerweile ist diese nicht nur in den Nachbarländern angekommen, sondern dringt auch in Europa vor.
Je länger die Pandemie dauert, desto mehr Mutationen finden statt, und je mehr sich das Virus verändert, desto wahrscheinlicher wird es, dass der Schutz durch die jetzigen Impfstoffe abnimmt. „Die einzige Möglichkeit, dies zu verhindern, ist die faire Verteilung von Impfstoffen an alle Länder“, ist Tedros Adhanom Ghebreyesus, Chef der Weltgesundheitsorganisation WHO, überzeugt.
Serum für Covax und die Welt
Und hier geht der Blick wiederum nach Indien, denn das Land ist derzeit nicht nur das Epizentrum des Problems, sondern auch ein wichtiger Teil der Lösung. Mit dem Serum Institute of India beheimatet es nämlich den größten Impfstoffhersteller der Welt, fast zwei Drittel aller Kinder weltweit werden mindestens einmal im Leben mit einem Impfstoff aus der westindischen Wirtschaftsmetropole Pune etwa gegen Polio, Masern oder Diphterie geimpft. Und während in den vergangenen Monaten vielerorts Hersteller an ihre Grenzen gerieten, gelingt dem Weltmarktführer in Indien seine aktuelle Hauptaufgabe, in kürzester Zeit große Mengen Covid-Impfstoff zu produzieren, bislang recht gut – mehr als zwei Millionen Dosen AstraZeneca sind es pro Tag.
Die in Pune produzierten Impfstoffe sollten ursprünglich in alle Welt geliefert werden. Doch angesichts der dramatischen Lage im Land stoppte die indische Regierung die Impfstoffexporte im März bis auf weiteres. Insbesondere für die globale Impfstoffinitiative Covax, die der indische Hersteller bis dahin fast im Alleingang beliefert hatte, bedeutete der Exportstopp einen herben Rückschlag. Bis Sommerbeginn fehlten Covax allein dadurch etwa 190 Millionen Impfdosen. Und der CEO des Serum Institute, Adar Poonawalla, schätzt, dass die Lieferungen erst gegen Ende des Jahres wieder aufgenommen werden können.
Daten und Fakten
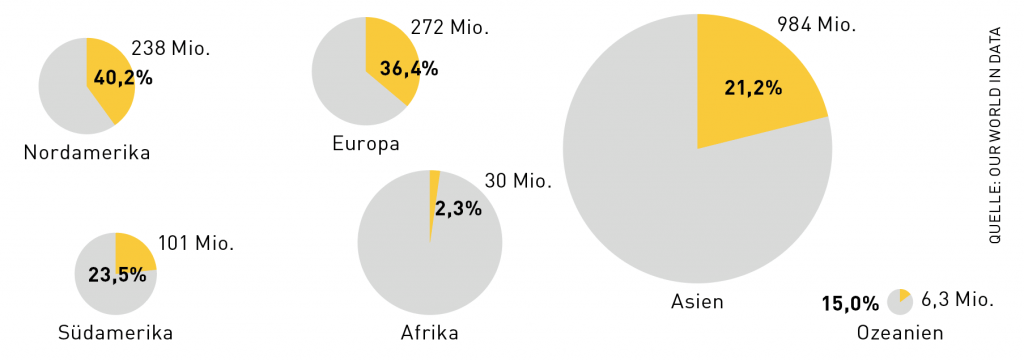
Ungleich große Aufgabe
Während in Nordamerika relativ gesehen die meisten Menschen zumindest einmal geimpft sind, führt der bevölkerungsreichste Kontinent Asien in absoluten Zahlen. Grundsätzlich hängen die ärmeren Staaten den Industrieländern deutlich hinterher.
Riesenprojekt Covax
Covax – ein Kürzel für Covid-19 Vaccines Global Access – wurde bereits im April 2020 von der WHO, der Impfallianz Gavi sowie dem Forschungsverbund Coalition for Epidemic Preparedness Innovations CEPI ins Leben gerufen. Das ambitionierte Ziel: rund ein Viertel der Weltbevölkerung, insbesondere das Gesundheitspersonal sowie die ältesten und schwächsten Menschen, bis Ende des Jahres 2021 mit einer Covid-Impfung zu versorgen.
192 Staaten schlossen sich der Initiative an, wobei reichere Staaten, die ihren Impfstoffbedarf meist über bilaterale Abkommen decken, die Initiative zugunsten der Entwicklungsländer unterstützen. Mit zugesagten vier Mrd. Dollar sind die USA der größte finanzielle Geber, gefolgt von Deutschland, das rund zwei Mrd. Euro in Aussicht stellte, und Großbritannien. Die EU ist der viertgrößte Geber. Spenden kommen auch von privaten Einrichtungen wie der Gates Stiftung. Die ärmeren Staaten sollen so vergünstigte oder kostenlose Impfstoffe erhalten – 92 Entwicklungsländer gelten als förderungswürdig.
Covax unterstützte die Pharmaunternehmen beim beispiellos schnellen Entwicklungs- und Produktionsprozess der Impfstoffe durch Anreize und Abnahmegarantien und konnte in der Folge deutlich bessere Konditionen aushandeln, als es einzelnen finanzschwachen Entwicklungsländern je möglich gewesen wäre. Das Kinderhilfswerk der Vereinten Nationen Unicef, das jährlich Millionen Kinder weltweit etwa gegen Masern oder Polio impft, wurde mit der Durchführung dieser größten Impfkampagne der Geschichte beauftragt.

Impfsprint in den Bergen
Im kleinen Himalaya-Königreich Bhutan wurde Rekordverdächtiges geleistet: Ende März und Anfang April wurden innerhalb weniger Tage mehr als zwei Drittel der Bevölkerung mit einer Dosis Astra Zeneca gegen Covid-19 geimpft. Dafür wurden in dem unwegsamen 750.000-Einwohner-Staat 1.200 Impfstationen über das Land verteilt eingerichtet. Möglich machte die schnelle Durchimpfung aber vor allem der große Nachbar Indien, der Bhutan die Impfstoffe bereits im Jänner zur Verfügung gestellt hatte. Der indische Exportstopp trifft nun aber auch Bhutan, dessen Bewohner auf die zweite Dosis warten. Es gibt jedoch Signale, dass die Schweiz die benötigten Dosen spenden könnte.
Millionenfacher Nachschub für Covax
Welche Räder lassen sich noch drehen, damit Entwicklungsländer bei der Deckung ihres Impfbedarfs so rasch wie möglich vorankommen? Zum einen haben die Pharmaunternehmen angekündigt, Covax massenhaft Impfstoffe zum Selbstkostenpreis zu überlassen. BioNTech und Pfizer etwa haben zugesagt, bis Ende des Jahres eine Milliarde Dosen zur Verfügung zu stellen. Zum anderen gibt es seitens der Industrieländer die Bereitschaft, überschüssige Impfdosen zu spenden. Viele von ihnen haben deutlich mehr Impfstoff geordert, als sie für die Immunisierung der Bevölkerung benötigen (so hat Kanada sechsmal mehr Dosen bestellt, als es Einwohner hat, in Österreich liegt die Impfstoffabdeckung bei etwa 230 Prozent). Zudem gab die deutsche Bundeskanzlerin Angela Merkel am Rande des G7-Gipfels im englischen Cornwall bekannt, dass die sieben großen Industriestaaten bis Ende 2022 2,3 Milliarden Impfdosen an ärmere Länder spenden werden.
Zusätzlich werden die G7 das Covax-Dachprogramm, den ACT-Accelerator, finanziell stärken. Dieser stellt ärmeren Staaten neben Impfungen auch Diagnostika und Therapeutika zur Verfügung. Derzeit fehlen rund 13 Mrd. Euro, um die für heuer geplanten Vorhaben durchzuführen. Laut einer aktuellen Studie der Internationalen Handelskammer stehen die benötigten Geldmittel in keinem Verhältnis zu den Kosten, die die Weltwirtschaft zu tragen hätte, falls sich die Infektionen in Schwellen- und Entwicklungsländern unvermindert ausbreiteten. Die volle Kapitalisierung des ACT-Accelerator sei demnach „ein klarer Investment-Case“.
Covax hat Sand im Getriebe
Die erste Covax-Impfdosis erhielt am 24. Februar Nana Akufo-Addo. Akufo-Addo ist kein Mitarbeiter im Gesundheitsbereich, sondern der Präsident Ghanas. Mit seiner Impfung wolle er seinen Landsleuten mit gutem Beispiel vorangehen, so seine Worte. 600.000 vom Serum Institute produzierte Dosen des Herstellers AstraZeneca hatte das Flugzeug nach Accra an Bord, noch am ersten Tag wurden in Ghana 100.000 Menschen geimpft.
Wegen der ausbleibenden Dosen aus Indien warteten viele der Erstgeimpften jedoch vergeblich auf ihre zweite Dosis. „Wir haben durch Spenden und Umverteilungen noch einige Dosen nach Ghana schicken können, aber das ist zu wenig“, berichtet Covax-Koordinator Benjamin Schreiber. Mitte Juni hatte Covax in Summe rund 83 Millionen Impfdosen in 131 Länder geliefert. Christoph Strupat, Gesundheitsexperte beim Deutschen Institut für Entwicklungspolitik DIE, zieht eine Zwischenbilanz: „Bislang blieb Covax deutlich hinter den Erwartungen und Zielen zurück.“
Interview mit Benjamin Schreiber, Covax-Koordinator
Montageplan für Impf-Ikeas
Ausbau der Produktion
Letztlich wird man aber auch nicht darum herumkommen, die Produktion deutlich auszubauen. In den vergangenen Jahren erreichte die globale Impfstoffnachfrage ein Volumen von drei bis fünf Milliarden Dosen, heuer liegt der Bedarf bei zusätzlichen zwölf Milliarden Covid-Impfstoffdosen – eine rein privatwirtschaftlich kaum lösbare Steigerung.
Afrikanischer Vorreiter
Marokko impfte im Frühjahr schneller als die meisten europäischen Staaten und hat im innerafrikanischen Vergleich mit Abstand die meisten Menschen geimpft. Bis Mitte Juni wurden rund 25 Prozent der knapp 40 Millionen Einwohner mit zumindest einer Dosis versorgt. Die WHO feierte das Königreich als „Musterbeispiel“ für eine erfolgreiche Impfkampagne, etwa weil das Land frühzeitig auf mehrere Anbieter gesetzt hat und eine funktionierende digitale Plattform die schnelle Vergabe der Termine erlaubt. Wegen des indischen Exportstopps hat aber auch die marokkanische Impfkampagne zuletzt deutlich an Tempo eingebüßt.
Die in diesem Kontext teilweise heftig geforderte Aufhebung des Patentschutzes für Covid-19-Impfstoffe erweist sich bei näherem Hinsehen jedoch nicht als erfolgversprechendes Mittel, um der aktuellen Impfstoffknappheit zu begegnen. Auslöser der Debatte war der bei der Welthandelsorganisation WTO eingereichte Antrag Südafrikas und Indiens auf Aufhebung des TRIPS-Abkommens über Rechte des geistigen Eigentums für Covid-Impfstoffe. Mehr als hundert WTO-Mitgliedsstaaten unterstützten den Vorstoß, um zu erreichen, dass jegliche Hersteller zugelassene Covid-Impfstoffe herstellen dürfen. Das Argument: Nur so ließen sich die für eine rasche Durchimpfung der Weltbevölkerung benötigten Produktionskapazitäten kurzfristig bereitstellen.
Die meisten Industriestaaten winkten umgehend ab, Pharmaunternehmen argumentieren, dass nur dank der 20 Jahre geltenden Patente die hohen Investitionen für die Impfstoffforschung überhaupt refinanziert werden könnten. Auf eine einfache Formel gebracht: Ohne Patente kein Fortschritt. Zuletzt hat sich aber auch die USA für ein Aussetzen des Patentschutzes ausgesprochen – wohlgemerkt, erst nachdem die eigene Bevölkerung auch aufgrund eines strikten Exportstopps, der etwa zu Engpässen in Indien geführt hat, äußerst rasch mit Impfstoffen versorgt werden konnte und die heimische Nachfrage nun fast erloschen ist. Auch Frankreich schloss sich den amerikanischen Forderungen an, die EU-Kommission signalisierte zudem Gesprächsbereitschaft.
Befürworter einer Aufhebung des Patentschutzes stellen immer wieder die Analogie zum Kampf gegen HIV/AIDS in den 1990er Jahren her. Die neuartigen HIV-Medikamente retteten damals in den Industrieländern vielen Menschen das Leben. Vor allem in Afrika, wo die Krankheit am schlimmsten wütete und dies bis heute tut, waren diese Medikamente für die allermeisten aber unbezahlbar. Millionen Menschen starben. Die südafrikanische Regierung unter Nelson Mandela setzte sich damals über die Patentschutz-Regelungen hinweg und ließ von indischen Pharmafirmen Generika produzieren. Es folgte eine Klage der Pharmaunternehmen, die sie aufgrund des riesigen Imageschadens, der damit einherging, letztlich zurückzogen. Generika für HIV-Medikamente wurden daraufhin grundsätzlich akzeptiert und die Preise sanken von etwa 10.000 auf nur noch 150 Dollar für die Behandlung einer erkrankten Person.

Erleben wir nun eine Neuauflage des damaligen Konflikts? Nur auf den ersten Blick ist die Situation wirklich vergleichbar. Impfstoffe erfordern nicht nur deutlich mehr und kostenintensivere Forschung als Medikamente, ihre Produktion ist auch wesentlich komplizierter als etwa jene der HIV-Tabletten. Es liege also nicht an den Lizenzen, dass der Covid-Impfstoff knapp sei, betonte kürzlich der operative Geschäftsführer von BioNTech Sierk Poetting gegenüber der Wochenzeitung „Die Zeit“. Allein angesichts des komplizierten Produktionsverfahrens sowie fehlender Rohstoffe sei es gar nicht möglich, dass ein Unternehmen in Afrika innerhalb weniger Monaten eine Produktion des Impfstoffes hochfahre. Auch mit Blick auf notwendig werdende Anpassungen der Impfstoffe an neue Virusmutationen scheint eine Aufhebung des Patentschutzes nur bedingt zielführend. Ökonom Gabriel Felbermayr, der im Herbst die Leitung des Österreichischen Instituts für Wirtschaftsforschung WIFO übernimmt, sprach gegenüber dem Magazin „Der Spiegel“ von einem „sehr problematischen Signal“, das von der Forderungen nach einer Aufhebung des Patentschutzes ausgehe: „Hunderte Unternehmen haben viele Milliarden Euro in Forschung investiert; nur wenige waren erfolgreich. Für die Branche ist es notwendig, dass im Durchschnitt erwartet werden kann, dass sich Forschung lohnt“, so Felbermayr.
Christoph Strupat vom DIE hält die gesamte Polarisierung für wenig zielführend und plädiert für einen differenzierten Blick auf die Situation – und die verfügbaren Impfstoffe: „Eine Patentschutzaufhebung würde bei dem neuartigen mRNA-Impfstoff in der Tat nicht viel bringen. Es gibt aber auch neben dem Serum-Institut einige weitere Unternehmen in Indien, die die vektorbasierten Impfstoffe, also jene von Johnson&Johnson und Astra Zeneca herstellen können.“
Mittelfristig brauche es jedenfalls einen Mittelweg zwischen dem Status Quo und der Aufhebung des Patentschutzes. Viele Wissenschaftler begrüßen dabei laut Strupat die aus Costa Rica stammende Idee namens C-Tap (Covid-19 Technology Access Pool): ein Patent- und Wissenspool, der zu mehr Kooperation zwischen den Herstellern anregen soll. Dabei ist es mitnichten so, dass die aktuelle Krise nicht bereits zu mehr Zusammenarbeit geführt hätte. Laut dem Internationalen Handelsverband der Pharmaunternehmen haben Pharmafirmen insgesamt 280 Partnerschaftsverträge über die Produktion von Covid-19-Impfstoffen abgeschlossen – etwa drei Viertel dieser Verträge beinhalten einen Technologietransfer.
Impfstoffe aus der Karibik

Kuba ist eines der wenigen Entwicklungsländer, das mit Impfstoffen und Medizintechnik aus eigener Produktion von sich reden macht. Das Land forscht zurzeit an fünf potenziellen Covid-19-Impfstoffen. Soberana-2, Kubas fortgeschrittenster Impfstoffkandidat, befindet sich bereits in Phase drei der klinischen Studien. Die kubanische Regierung hofft, dass sie davon bis zum Ende des Jahres 100 Millionen Dosen produzieren kann. Impfstoffe, die am Heimmarkt nicht benötigt werden, sollen an Verbündete wie Venezuela verkauft werden. Der sozialistische Inselstaat kann bei der Entwicklung und beim Export von Impfstoffen auf eine lange Erfahrung zurückblicken.
Post-Covax: Impfstoffe Made in Africa
Perspektivisch soll auch in Afrika eine eigene Pharmaindustrie entstehen. Bei einer eigens organisierten Konferenz haben zahlreiche afrikanische Regierungschefs erst kürzlich betont, dass die Impfstoffproduktion in Afrika auf eigene Beine gestellt werden solle. Strupat zeigt sich angesichts solcher Ankündigungen allerdings verhalten optimistisch: „Rund um die Aids- oder Ebola-Krise wurde ebenfalls signalisiert, man wolle eine afrikanische Produktion aufbauen. Geschehen ist nichts. Man kann nur hoffen, dass ein solcher Prozess durch eine Pandemie dieses Ausmaßes jetzt doch und nachhaltig in Gang kommt.“
Seitens der EU wird ein solches Ansinnen gerne unterstützt. Sie hat kürzlich angekündigt, sich mit einer Mrd. Euro am Aufbau von Impfstoff-Produktionsstätten in Afrika zu beteiligen. Damit sollen bis 2040 mehr als die Hälfte der in Afrika eingesetzten Impfstoffe in mehreren Produktionsstandorten am Kontinent selbst hergestellt werden. Mit diesen Bestrebungen verbindet sich auch die Hoffnung, dass durch die neuartige mRNA-Technologie die Suche nach einem hochwirksamen Malariaimpfstoff endlich an ihr Ziel gelangt.
Neben Südafrika zeigen sich Kenia, Senegal, Ghana und Ruanda am Aufbau einer Impfstoffproduktion im eigenen Land besonders interessiert. Laut Strupat ist das kein Zufall, da gerade diese Länder aufgrund des gestiegenen Wohlstands von der gemeinnützigen Impfallianz Gavi nicht mehr beliefert werden. Womit er die Grenzen einer kostenlosen Impfstoffversorgung aufzeigt: „Man muss leider sagen, dass Gavi und letztlich auch die Covax-Initiative den Bemühungen um den Aufbau einer lokalen Produktion entgegenstehen. Für die Industrie ist der Impfmarkt in Afrika nun einmal ein ‚Gavi-Markt‘, also spendengetrieben.“ Solange sich daran nichts ändere, lohne es sich für Unternehmen nicht, in den Aufbau von Produktionsstätten oder die Erforschung von Impfstoffen zu investieren.
Etwas zu früh gefreut
In Chile hatten Mitte Juni bereits mehr als 60 Prozent der Bevölkerung die erste Impfdosis gegen Covid-19 erhalten. Entscheidend für die effiziente Impfkampagne war einerseits die frühe und seither kontinuierliche Verfügbarkeit von Impfstoffen. „Es gibt vor allem aber auch eine gut funktionierende Infrastruktur mit einem engmaschigen Netz an Impfzentren, wo unbürokratisch und nach Risiko- bzw. Altersgruppenzuordnung geimpft wird“, berichtet der Wirtschaftsdelegierte in Santiago de Chile, Drazen Maloca. Trotz des schnellen Impffortschritts kam es im April zu einer zweiten Covidwelle, die sogar deutlich gravierender ausfiel als die Erste. Das könnte auch mit dem Impferfolg selbst und einer verfrühten Lockerheit im sozialen Verhalten zusammenhängen.
Covax ist nicht das einzige Zeichen der Hoffnung
Die Pandemie ist eine gewaltige Bewährungsprobe und der Kampf gegen das Virus eine logistische Herausforderung für jeden einzelnen Staat dieser Welt. Dabei haben auch etliche Schwellen- und Entwicklungsländer von Marokko bis Bhutan Beachtliches geleistet. Und auch in Indien geht es langsam aufwärts: Während die Infektionszahlen sinken, sind mehr als 200 Millionen Inder zumindest einmal geimpft.